32 yrs old male with abdominal pain and vomitings
THIS IS AN ONLINE E LOG BOOK TO DISCUSS OUR PATIENT'S DE - IDENTIFIED HEALTH DATA SHARED AFTER TAKING HIS / HER /GUARDIAN'S SIGNED INFORMED CONSENT .HERE WE DISCUSS OUR INDIVIDUAL PATIENT'S PROBLEMS THROUGH SERIES OF INPUTS FROM AVAILABLE GLOBAL ONLINE COMMUNITY OF EXPERTS WITH AN AIM TO SOLVE THOSE CLINICAL PROBLEMS WITH COLLECTIVE CURRENT BEST EVIDENCE BASED INPUT
This is a case of 32 yr old male resident of nagaram , housekeeper in a hospital in kachiguda came to general medicine OPD with
CC: patient came to OPD with cheif complaints of abdominal pain , vomiting, Sob since 5 days.
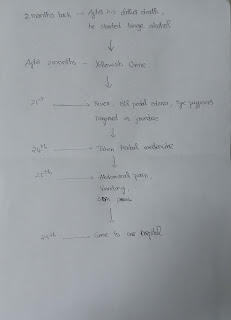
HOPI : patient was apparently asymptomatic 10 days back then he developed fever without chills and rigor , with no diurnal variation , yellowish urine without burning micturition , b/l pedal edema upto ankle , facial puffiness , for which he has gone to rmp and diagnosed as jaundice, later on 24 th he took a herbal medicine, and on 25 he developed abdominal pain which is sudden in onset and gradually progressive , squeezing type ,no aggregating factors and relieved on walking , vomiting 2 to 3 episodes per day which is bilious , non projectile associated with abdominal pain , Sob since 5 days, insidious in onset and gradually progressive, grade 4 type .
PAST HISTORY
2 months back his father died and in the family gathering he started binge alcohol consumption for 2 months with little consumption of food, later he developed yellowish urine and constipation.
Not a k/c/o hypertension, diabetes, thyroid, tb, epilepsy, asthama .
FAMILY HISTORY:
no relavent family history.
Drug history:
5 days back he took a dose (50 ml ) of herbal medicine
PERSONEL HISTORY:
Daily routine
He wakes up at 5:30 am and do his morning routine, eats breakfast at 7:00 am , usually he eats idli , dosa and goes to work ( housekeeper in hospital) , lunch at 1:00 pm , after his duty he returns to his home by 7:00 pm , eats dinner at 8:00 pm goes to bed at 10: 00 pm .
Diet : Mixed
Appetite : adequate
Sleep : adequate
Bowel and bladder : regular
Addictions - drinks alcohol since 9 years
Gutka ( ambar ) consumption - occasionally
FAMILY HISTORY: no relavent family history.
GENERAL EXPLANATION:
pt is conscious, coherent, cooperative and we'll oriented with time,place,person
Pallor:. No
ICTERUS: PRESENT
Cyanosis: Absent
Clubbing: Absent
Lymphadenopathy: No
Pedal edema: Absent
VITALS:
TEMP: 98.5 F
PR: 122 bpm
RR: 22 cpm
BP: 110/80
SYSTEMIC EXAMINATION:
ABDOMINAL EXAMINATION:
INSPECTION:
Mild distension
Scaphoid abdomen , no engorged veins , inverted umbilicus
PALPATION:
Tenderness in umbilicus, epigastrium, hypogastrium region
PERCUSSION:
dull note on right hypochondrium
AUSCULTATION:
Bowel sounds are heard
Cardio vascular examination:
No visible pulsations, scars, engorged veins. No rise in jvp
Apex beat is felt at 5 Intercoastal space medial to mid clavicular line.
S1 S2 heard . No murmurs.
Respiratory system :
Shape of chest is elliptical, b/l symmetrical.
Trachea is central. Expansion of chest is symmetrical
Bilateral Airway Entry - positive
Normal vesicular breath sounds
CNS examination:
No neurological deficit found.
Gait: normal.
Normal speech.
INVESTIGATION:
1)USG:
2)HEAMOGRAM:
3) COMPLETE URINE EXAMINATIO
4)SERUM CREATININE:
5)BLOOD UREA
6)SERUM ELECTROLYTES and SERUM CALCIUM
7)LIVER FUNCTION TEST:
ECG :
Provisional diagnosis
Jaundice , Aki
Alcoholic hepatitis ?
Acute liver injury? Hepatic encephalopathy?
TREATMENT:
ON 29/11/22
1)IV RL AND IV NS(75ML/HR)
2)INJ PANTOP 40MG/IV/OD
3)TAB UDILIV 300MG/PO/BD
4) HEAD END ELEVATION UPTO 30
5)INJ THIAMINE 1amp IN 100ML NS/IV/TID
6)INJ MONOCEF 1GM/IV/BD
7)SYP LACTULOSE 10ML/PO/BD
8)I/O CHARTING
9)TEMP CHARTING 4TH HOURLY
10)MONITOR/VITALS
ON 30/11/22
1) IVF RL AND NS(75ML/HR)
2)INJ PANTOP 40MG/IV/OD
3)INJ MONOCEF 1GM/IV/BD
4)TAB.UDILIU 300MG/PD/BD
5)TAB.ZOFER 4MG/PO/SOS
6)INJ THIAMINE 1AMP IN 100ML/NS/IV/OD
7)SVP LACTULOSE10ML/PO/BD
8)STRICT ZLOCHARANG
9)TEMP CHARANG4TH HRLY









Comments
Post a Comment