35 year old male came with C/o occasional palpitations and SOB since 3 months.

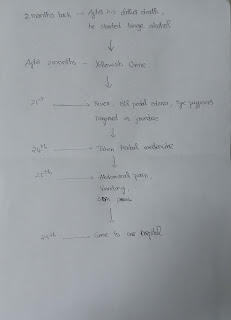
This is an online elog documenting de-identified patient health data after taking his signed consent to enforce a greater patient centered learning. DEIDENTIFICATION - The privacy of the patient is being entirely conserved. No identifiers shall be revealed through out the piece of work whatsoever. CASE DISCUSSION - 35 year old male came with C/o occasional palpitations and SOB since 3 months. HOPI- Patient was apparently asymptomatic 3 months back, then started developing occasional palpitations, relieved on consuming alcohol, not a/w chest pain. He developed SOB since 3 months, Grade 2, insidious in onset, gradually progressive, no aggravating and relieving factors. C/o decreased appetite since 2 months. C/o generalised weakness since 10 days. No H/o orthopnea and PND. No C/o fever, decreased urine output, burning micturition, pedal edema. PAST HISTORY- Not a k/c/o DM, HTN, CVA, CAD, TB, Epilepsy. PERSONAL HISTORY- Addictions- Patient is a regular drinker since last 15-16 yrs,